After recently feeling under the weather, including experiencing classic COVID-19 symptoms such as sore throat, the author finally decided to face her fears by stepping inside a hospital’s ER to have herself tested for COVID-19. Physically and mentally strong as well as impervious to fears from such routine medical procedures as blood extraction, she nevertheless felt the scare of her life while waiting for test results to come out.
By Hermes Joy S. Tunac
It all started one Thursday afternoon.
Two hours before finishing my work at the office, I decided to have my second cup of latte before working on a pending article. Halfway through my cup, I suddenly felt an itch in my throat. I ignored it at first, thinking that maybe it was just due to the the milk I used, which was different from my usual.
Hours had passed, but the itch in my throat persisted. I took immediate care as soon as I got home by gargling warm water with salt. Could it be you know what? By this time, I was already feeling slightly nervous, but still, I tried to stay calm. I went to bed early that night to rest and hopefully ease the discomfort I was feeling.
Come Friday morning, my situation worsened. My throat was not just itchy. It now felt heavy and sore. I immediately isolated myself from the rest of my family by staying inside my bedroom. At this point, I was already paranoid, since, as you may already know by now, a sore throat is one of the early symptoms of coronavirus infection or COVID-19, alongside colds, dry, persistent cough and fever.
If there’s no pandemic lurking outside our homes, I would have normally brushed such thoughts aside. I would have opted to simply rest at home for a day or two while resorting to common home remedies until my condition improved. No big deal, really. But that wasn’t the case. The clear and present danger of contracting COVID-19 and passing it on to other people, friends and loved ones included, is there. In short, the implications are far too big to imagine and simply ignore–isolation, contact tracing, untold expenses and the prospect of getting sick and eventually being wheeled to the ICU are no longer remote possibilities should I turn out COVID-19 positive.
Even before undergoing a test and finding out the result, I lost no time informing my colleagues whom I had close contact with for the past several days at the office about my condition. Our managing editor got our office disinfected as soon as he learned about it, and our team decided to work from home for the next few days just to play safe.
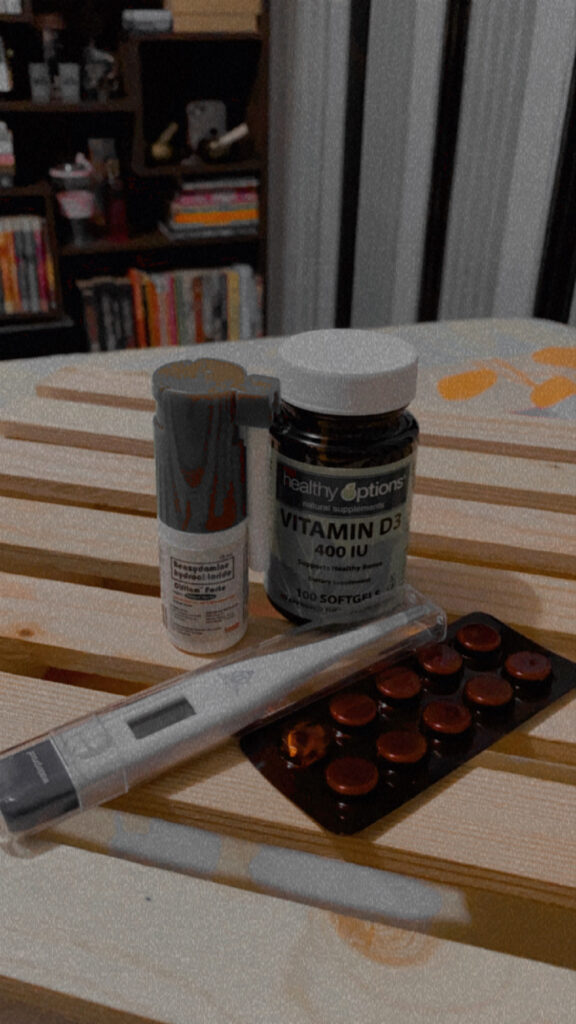
As I self-isolated inside my room, I just did what a paranoid person would perhaps most likely do in times of a pandemic—constant checking of temperature, drinking ginger tea as often as possible to soothe my sore throat, taking vitamins and supplements religiously and just thinking and trying out all sorts of distractions to keep my mind from dwelling on my paranoia.
The entire weekend passed, but I didn’t seem to be getting any better. In fact, to make matters worse, I already had cough and colds by Monday. That was when I finally decided to see a doctor. Initially, my plan was to visit a clinic to avoid big crowds in a hospital. I opted to go to The Medical City satellite clinic in BGC, but apparently, small clinics like them don’t normally entertain patients who are showing symptoms of COVID-19.
When the nurse at the clinic turned me away, my heart further raced through my chest. Do I have COVID-19? What should I do? Should I go home and continue going on self-medication? Or should I fight my fear and go straight to the hospital? These were the questions constantly going through my head that day. But my older brother JV, who is a registered nurse, convinced me to just go to St. Luke’s.
“Whether they test you or not, at least we won’t go home wondering anymore, and you’ll get a proper diagnosis,” he said.
My brother dropped me and my mom off at the hospital’s emergency department. All patients, whether experiencing COVID-19 symptoms or not, need to undergo the triage process just outside the ER.
Initial steps included sanitation, filling out of various forms–from basic bio-data to a more detailed medical and travel history–and temperature and blood pressure check. Prior to our hospital visit, I knew I didn’t have fever because I was constantly monitoring my temperature. That was one concern off my list. But to my surprise, when the nurse checked it again, my temperature hovered at 37.8 °C. My mom and I initially blamed it on the piping hot ramen because my temperature was normal the last time I checked, which was just before having lunch. Of course, in hindsight, the ramen had nothing to do with it.
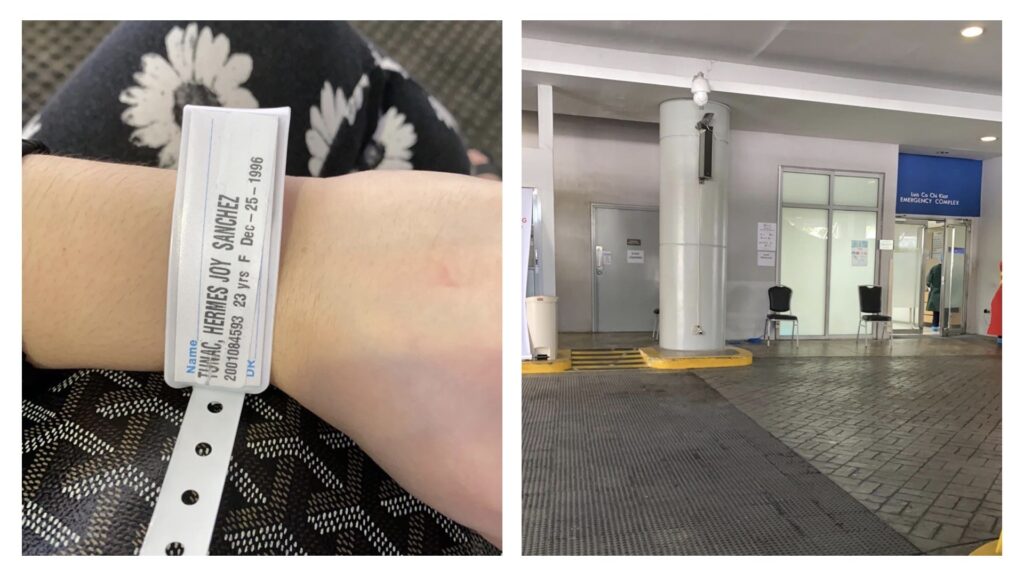
The doctor immediately led me to the other side of the room, together with other symptomatic patients. By this time, I was already considered a likely COVID-19 sufferer. In other words, I needed to undergo a complete blood count (CBC) and swab test to disprove that I was not.
With my active lifestyle and intuitive diet, I know I could recover fast had I tested positive. I know I have a strong immune system. At least, that was what I liked to believe. But just the thought of testing positive made me weak since there was still a chance, even if slightly, for me to go through untold suffering, even die from this novel coronavirus.
I’ve never been afraid of needles, or any laboratory tests that not a few people dread. So, I didn’t have any problems with blood extraction. But it was going to be my first time to do a swab test. Fear of the unknown slowly started to creep in, as I wasn’t sure what was in store for me.
Swab test is currently the most credible laboratory test for determining whether or not a patient is COVID-19 positive. The process involves inserting a 6-inch long swab into the cavity between the nose and mouth. For the full test information, kindly refer below, as supplied to me by St. Luke’s Cellular Immunology and Immunogenetics department.
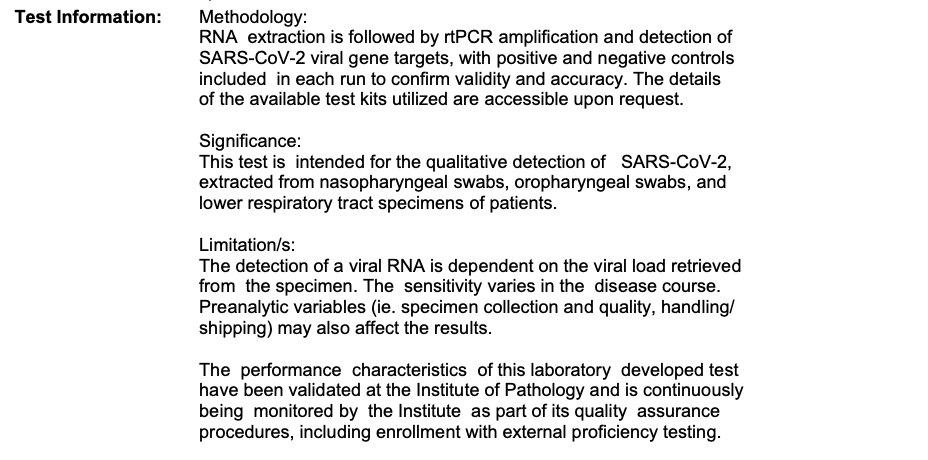
Prior to the main procedure, the nurse oriented me on what to expect during a swab test, which was the pain or discomfort that I might feel while the swab is physically inserted inside my cavity. She reminded me to stay calm so as not to prolong or complicate the procedure.
Much to my relief, the swab test only took less than a minute. My tolerance for pain, I’d like to believe, is high, so I only felt a slight discomfort during the actual insertion of the swab between my nose and mouth. But the tension I felt was at an all-time high. So much so that it was as if a thorn had been pulled from my side immediately after it was over.
A lot of articles are circulating online of how painful the swab test is. I was an unlikely victim for having read too much and believed such accounts. As far as I was concerned, the actual swabbing wasn’t so bad. But the agony of being left in the dark, not knowing how things would turn out, remained, as I had to wait for 24 to 48 hours for the result to come out.
After I underwent all the necessary laboratory tests, my doctor sent me home with instructions to isolate myself for 14 more days, increase fluid intake and proceed immediately to the nearest hospital’s emergency department if my situation worsens.
As soon as I reached home, I lost no time following doctor’s orders, spending all that time trying to make both my mind and body feel stronger, my disposition better. Apart from going on self-isolation, thanks to my mom, I never missed a meal or skipped my daily yoga workout. I continued taking prescribed medicines and vitamins religiously. With the help of rest, meditation and prayers, it didn’t take long before I soon felt well again even before receiving my swab test result.
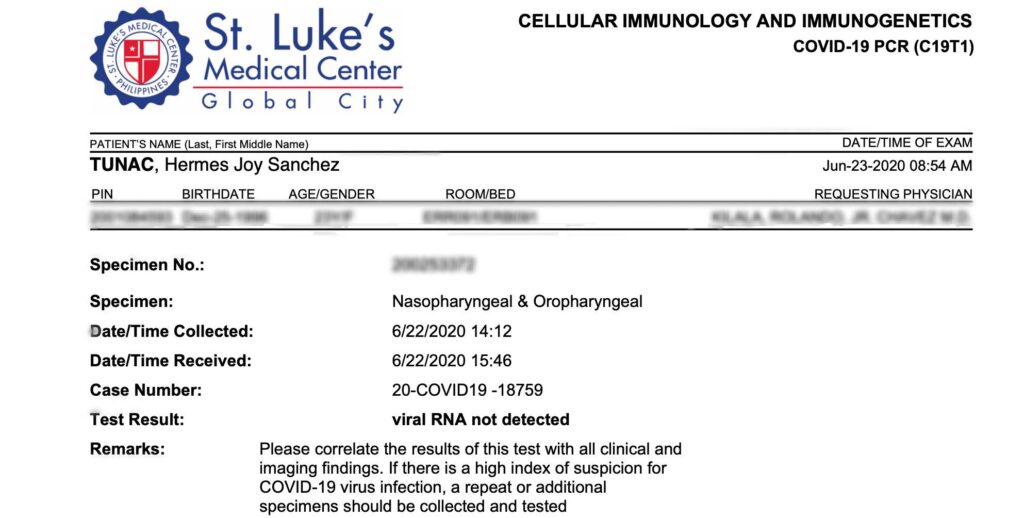
After three days of waiting, I felt an ultimate sense of relief to know that I was COVID-19 negative.
This whole experience of being a COVID-19 “suspect” has made me realize that health, despite the cliché, is really indeed wealth. The experience also made me more appreciative of life and humbler of the privileges I have, which afforded me to have myself tested, stay at home and recuperate with the support of my family.
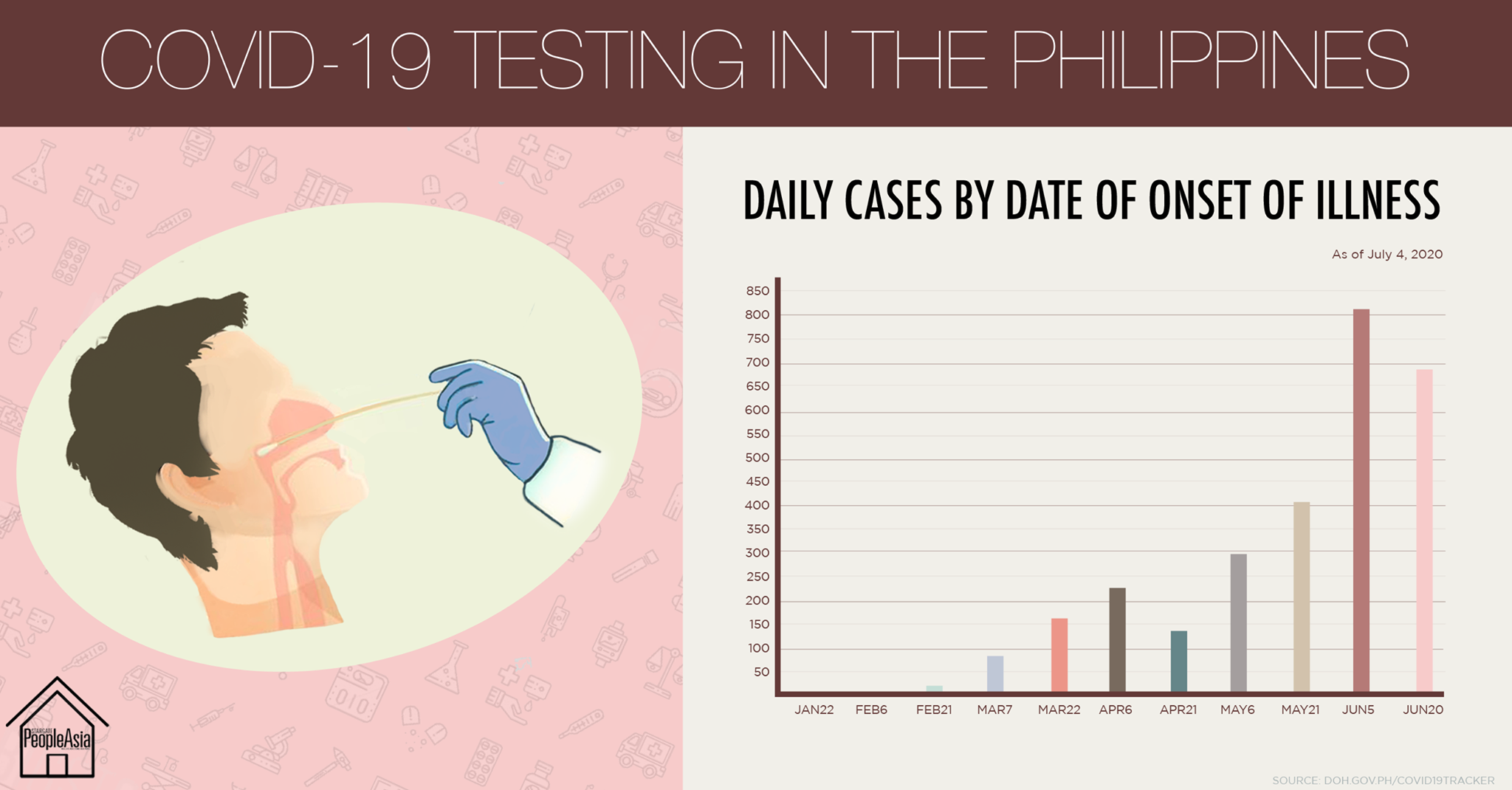
As of July 1, there are 71 licensed testing labs in the Philippines, including St. Luke’s BGC and QC, Makati Medical Center, Asian Hospital and Medical Center and The Medical City.
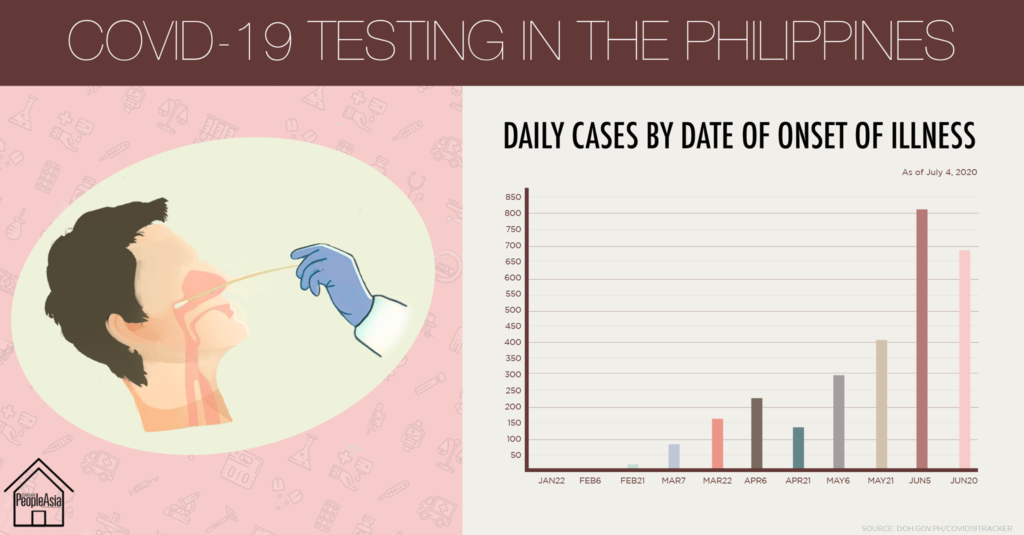
To know more details about COVID-19 in the Philippines, visit www.doh.gov.ph/covid19tracker.